Clinical features
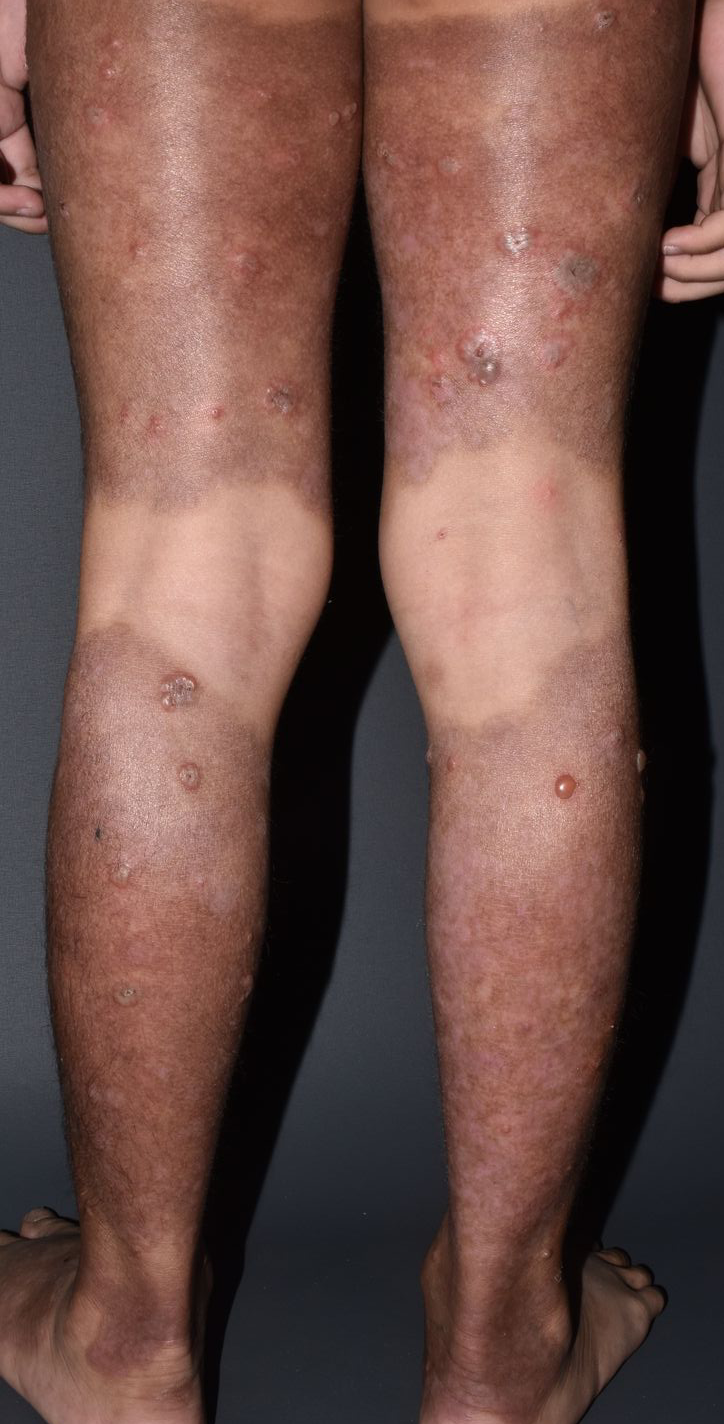
The lesions, which initially appeared as erythematous pruritic tense vesicles, first developed in his genital and inguinal areas five months prior to the consultation. These lesions rapidly spread to his trunk, extremities, scalp, and face, with spontaneous rupture and crusting. Three months prior to the consultation, a local physician diagnosed the patient with psoriasis and prescribed oral antibiotics and an unrecalled topical ointment. There was partial symptom resolution. However, one month before the consultation, the lesions worsened, requiring a five-day admission at a local hospital for an unspecified skin infection. The patient received unrecalled intravenous antibiotics, which provided slight improvement of the lesions. After discharge, a pediatrician prescribed oral prednisone, oral cefixime, and tar shampoo, which afforded partial symptom relief. Twenty days before we saw the patient at our Dermatology Clinic, a private dermatologist performed a skin punch biopsy on him, which revealed a subepidermal blistering disease compatible with linear IgA bullous dermatosis (LABD). He was then prescribed dapsone at a dose of 50 mg per day and immediately referred to us for complete work-up. The patient had no family history of similar skin diseases, autoimmune diseases, or malignancies, and no history of food or drug allergies. The patient had no recent fever, cough, colds, or abdominal or joint pain.Upon examination, there were multiple tense, clear, fluid-filled vesicles and bullae with erosions distributed on the scalp, face, trunk, extremities, and genital areas, some forming a “string of pearls” pattern, with areas of erosions topped with yellowish crusts, as well as hyperpigmented patches on previously affected areas (Figure 1 and 2). There were no oral or nasal mucosal lesions, nor lymphadenopathy.
Diagnostics, therapeutics, and outcomes
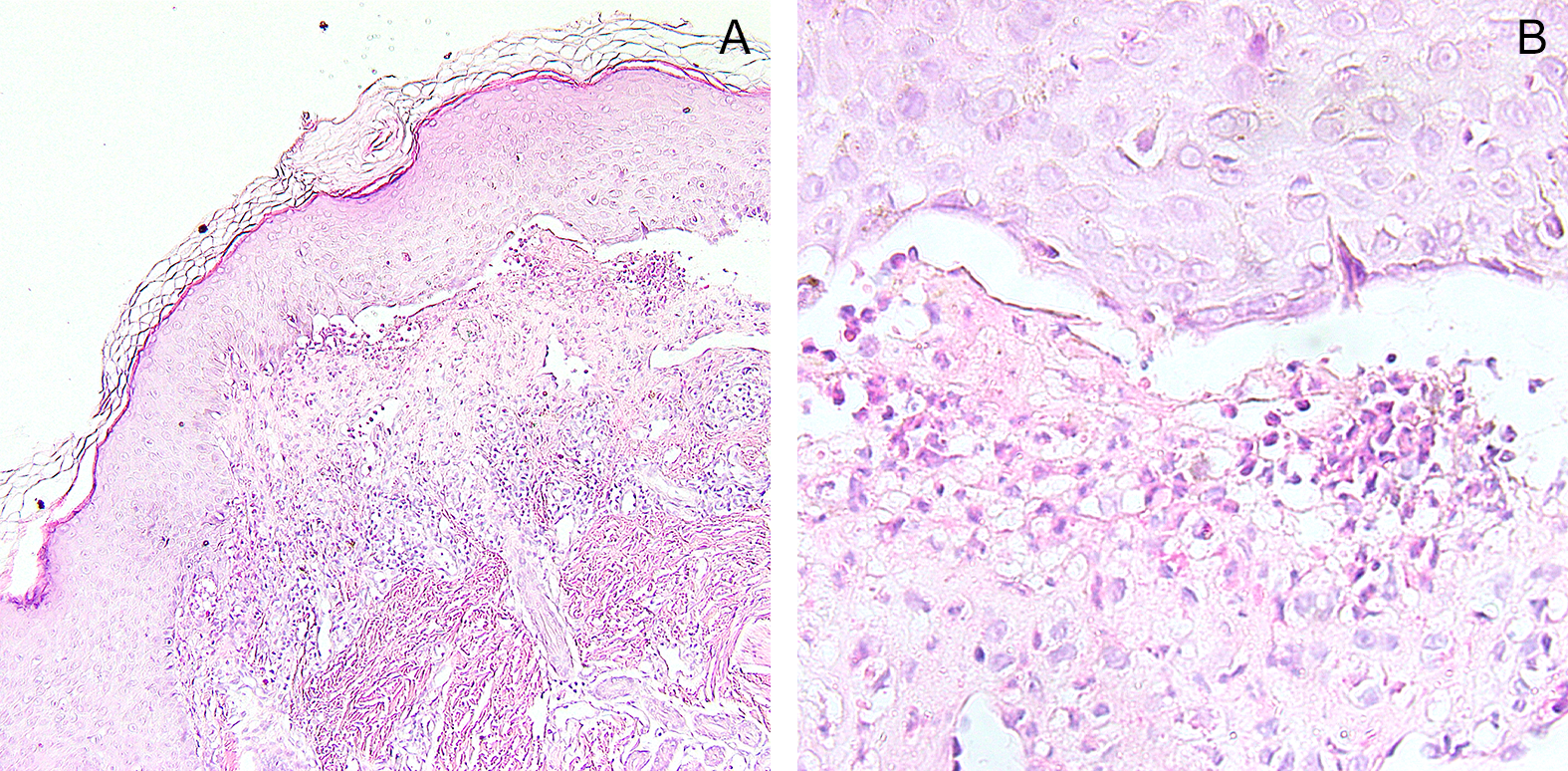
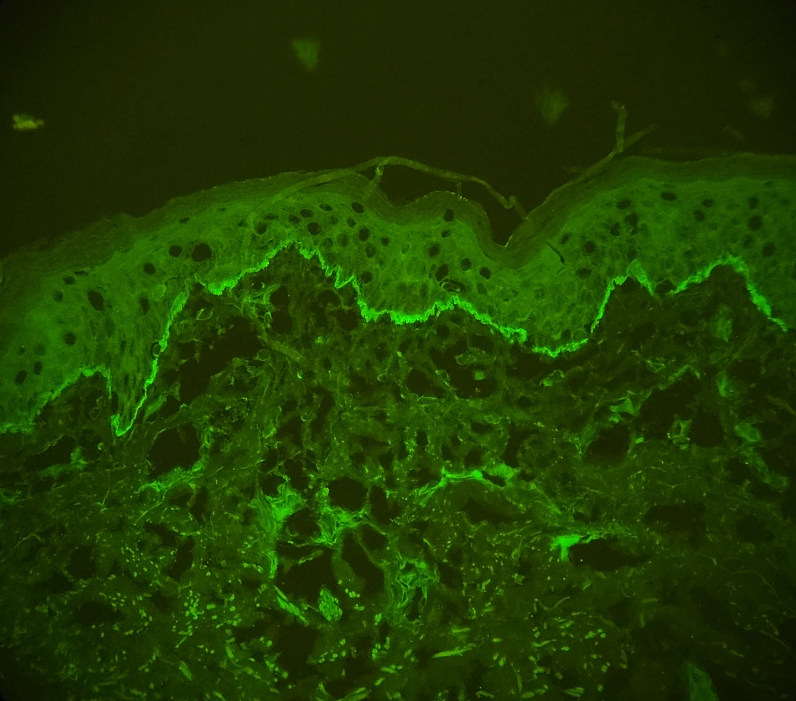
Hematologic and biochemical examinations, including a G6PD test, were unremarkable. A skin punch biopsy of an intact vesicle on the upper back revealed a subepidermal blister containing numerous neutrophils (Figure 3). A direct immunofluorescence (DIF) study performed on the perilesional area of the patient’s upper back showed strong linear IgA deposition along the basement membrane zone (Figure 4), confirming the diagnosis of LABD.We started the patient on dapsone at an initial dose of 1.4 mg/kg/day for two weeks and gradually increased the dose to 2.7 mg/kg/day. We also prescribed daily skincare with mild soap and emollients. This resulted in a dramatic symptom resolution and a decrease in new-onset lesions after four weeks of therapy (Figure 5). The patient and his family were counseled on the usual course of the disease, which may recur despite treatment, but generally has a good long-term prognosis, with remission usually achieved within two years.
The patient followed up every two weeks at the outpatient department, where clinical hemodynamic parameters such as blood pressure and pallor, along with laboratory tests including hemoglobin, reticulocyte count, and lactate dehydrogenase, were monitored to ensure tolerability to dapsone and to rule out any signs of hemolytic anemia or methemoglobinemia. After eight weeks of follow-up, the patient was able to tolerate the medication without any signs of adverse effects.