Characteristics and outcomes of non-traumatic out-of-hospital cardiac arrest during the COVID-19 pandemic: policy notes
SPMC J Health Care Serv. 2025;11(1):4 ARK: https://n2t.net/ark:/76951/jhcs3x8kw3
1Research Utilization and Publication Unit, Southern Philippines Medical Center, JP Laurel Ave, Davao City, Philippines
Correspondence Christine May Perandos-Astudillo, alleiandrah@gmail.com
Received 10 June 2025
Accepted 27 June 2025
Cite as Perandos-Astudillo CM, Roño RC. Characteristics and outcomes of non-traumatic out-of-hospital cardiac arrest during the COVID-19 pandemic: policy notes. SPMC J Health Care Serv. 2025;11(1):4. https://n2t.net/ark:/76951/jhcs3x8kw3
Introduction
The COVID-19 pandemic markedly affected the incidence and outcomes of OHCA worldwide. Regions with a high COVID-19 burden experienced an uptick in OHCA cases and a decrease in bystander-initiated cardiopulmonary resuscitation (CPR).3 Cardiac arrests increasingly occured at home, while incidence in public settings declined.4 Additionally, patients with chronic conditions often deferred their regular medical check-ups and avoided emergency departments (ED) for fear of infection. These factors--delays in emergency medical response, reduced bystander CPR, and limited health care services utilization--significantly undermined OHCA survival rates.5
This article aims to recommend health care policies informed by findings from a study conducted at a tertiary hospital in Davao City, examining the characteristics and outcomes of non-traumatic OHCAs during the COVID-19 pandemic.
Main evidence
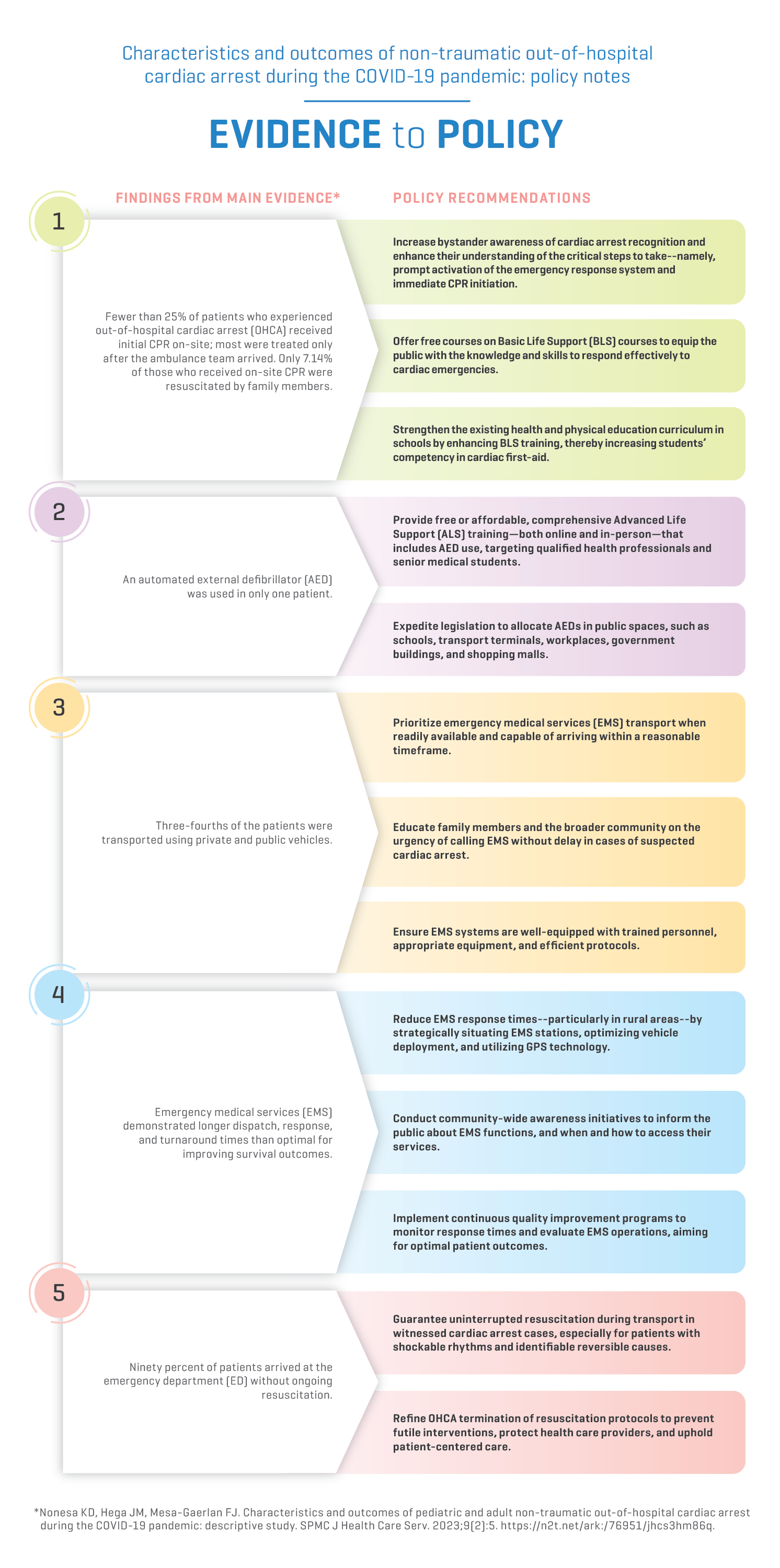
Policy recommendations based on these findings are outlined in the evidence-to-policy diagram below.
Evidence-to-policy diagram
Related evidence
Only a small proportion of patients experiencing OHCA receive bystander CPR on-site. Most are resuscitated only upon the arrival of ambulance personnel. During the pandemic, hesitancy among first responders to initiate CPR was noted,10 likely due to concerns about exposure and inadequate personal protective equipment (PPE). In 2021, the Department of Education issued the implementing rules and regulation for Republic Act 10871--the Basic Life Support Training in Schools Act--which integrates emergency cardiovascular care into the health and physical education curriculum of elementary and secondary schools.11
Raising public awareness of cardiac arrest signs and equipping bystanders with the knowledge and confidence to perform CPR are crucial. The timing of CPR initiation is the main factor influencing survival and recovery following an OHCA, rather than the technical skills of the individual administering it. Timely CPR, even if not perfectly executed, greatly enhances the likelihood of a favorable outcome compared to late CPR.12
EMS providers rely on AEDs, which detect shockable rhythms and deliver appropriate shocks. The presence of an initial shockable rhythm in OHCA is linked to better survival outcomes.13 14 15 To support early interventions, Public Access Defibrillation (PAD) systems place AEDS in public spaces such as airports, malls, and government buildings. These systems are associated with improved OHCA survival rates.16 However, timely AED access remains a challenge in low to middle-income countries (LMICs). In 2024, the Philippine Heart Association called on legislators to expedite legislation mandating AED availability in public spaces.17 Some local government units in Metro Manila have begun implementing PAD systems.18 Policies should also be formulated to improve public awareness of AEDs and encourage their use, which can be achieved through education, training, and strategic placement.16
In Vietnam, research suggests that non-EMS transport (e.g., private vehicles or taxis) is frequently used because it is perceived as faster and more accessible, especially in congested urban areas.19 EMS response may also take longer in rural or remote settings due to geographic and logistical constraints.20 While private transport can shorten time to hospital arrival, it may limit access to critical interventions during transit, unless bystanders are trained in life support techniques. Conversely, EMS crews can deliver Advanced Life Support (ALS), including CPR, defibrillation, and medications, provided they are properly equipped.19 However, one study found lower survival rates among patients transported by EMS compared to those using non-EMS transportation modalities.21 These findings highlight the importance of considering patient condition, transport timing, and local EMS capacity when determining the most effective mode of transport.
Longer dispatch, response, and turnaround times have a documented negative impact on survival rates. During the pandemic, many studies reported approximately one-minute delays in EMS response, partly due to time spent donning PPE.4 22 23 Each minute of delay reduces the likelihood of detecting a shockable rhythm by 8%.24 Shorter response times are consistently associated with better outcomes, including higher survival rates and reduced risk of neurological damage. Ideally, EMS should be dispatched immediately upon receiving the call, with a target response time of 6.5 to 8 minutes when bystander CPR is performed.25 26 Response time improvements may be achieved through protocol optimization and training,27 expanded AED accessibility, and technological solutions--such as GPS-based localization systems that alert first responders to episodes of fatal arrhythmia.28
Globally, OHCA survival remains low--ranging from 8-15.8% in a few high-income Western and Asia-Pacific countries,29 30 31 and dropping to 1-3% in many LMICs in Asia.32 33 For countries with developing EMS infrastructure like the Philippines, a multifaceted approach is essential. This includes strategic ambulance and PAD deployment, robust communication networks using GPS, and enhanced public awareness through community-based programs and mass media campaigns emphasizing early recognition, activation of emergency services, and high-quality CPR. Strengthening these pillars holds great promise for improving OHCA outcomes.
Contributors
CMPA, and RCR contributed to the conceptualization of this article. CMPA, and RCR wrote the original draft. Both authors performed the subsequent revisions, approved the final version, and agreed to be accountable for all aspects of this article and its corresponding infographic.
Article source
Commissioned
Peer review
Internal
Competing interests
None declared
Access and license
This is an Open Access article licensed under the Creative Commons Attribution-NonCommercial 4.0 International License, which allows others to share and adapt the work, provided that derivative works bear appropriate citation to this original work and are not used for commercial purposes. To view a copy of this license, visit https://creativecommons.org/licenses/by-nc/4.0/.
References
1 Ho AFW, Lim MJR, Earnest A, Blewer A, Graves N, Yeo JW, et al. Long term survival and disease burden from out-of-hospital cardiac arrest in Singapore: a population-based cohort study. Lancet Reg Health West Pac. 2022 Dec 28;32:100672.
2 Philippine College of Emergency Medicine - Pan-Asian Resuscitation Outcomes Study Group. SurVival from Out-of-Hospital Cardiac Arrests: Report of Resuscitation Outcomes and Modifiable Factors from a Philippine Emergency Medical Systems (EMS) Out-ofHospital Cardiac Arrest (OHCA) Registry [Internet]. Singapore Clinical Research Institute. [cited 27 June 2025]. Available from: https://www.scri.edu.sg/files/PAROS%20Presentations/24%20Aug%202016:%20Seoul,%20Korea/8_PAROS_Progress_Philippines_Dr_Faith_Aug_2016.pdf.
3 Baldi E, Klersy C, Chan P, Elmer J, Ball J, Counts CR, et al. The impact of COVID-19 pandemic on out-of-hospital cardiac arrest: An individual patient data meta-analysis. Resuscitation. 2024 Jan;194:110043.
4 Lim D, Park SY, Choi B, Kim SH, Ryu JH, Kim YH, et al. The Comparison of Emergency Medical Service Responses to and Outcomes of Out-of-hospital Cardiac Arrest before and during the COVID-19 Pandemic in an Area of Korea. J Korean Med Sci. 2021 Sep 13;36(36):e255.
5 Jokšić-Mazinjanin R, Marić N, Đuričin A, Rakić G, Srdanović I, Maljah M, et al. Out-of-hospital cardiac arrest before and during the COVID-19 pandemic: a retrospective observational study. Signa Vitae. 2024;20(11):68-74.
6 Nonesa KD, Hega JM, Mesa-Gaerlan FJ. Characteristics and outcomes of pediatric and adult non-traumatic out-of-hospital cardiac arrest during the COVID-19 pandemic: descriptive study. SPMC J Health Care Serv. 2023;9(2):5. https://n2t.net/ark:/76951/jhcs3hm86q.
7 Husain AA, Rai U, Sarkar AK, Chandrasekhar V, Hashmi MF. Out-of-Hospital Cardiac Arrest during the COVID-19 Pandemic: A Systematic Review. Healthcare (Basel). 2023 Jan 8;11(2):189.
8 American Heart Association. Out-of-hospital chain of survival [Internet]. Dallas: American Heart Association; 2024 [cited 2025 Jun 27]. Available from: https://cpr.heart.org/en/resources/cpr-facts-and-stats/out-of-hospital-chain-of-survival.
9 Scquizzato T, Landoni G, Paoli A, Lembo R, Fominskiy E, Kuzovlev A, et al. Effects of COVID-19 pandemic on out-of-hospital cardiac arrests: A systematic review. Resuscitation. 2020 Dec;157:241-247.
10 Sjöberg E, Wangel A-M. Ambulance personnel’s experiences of, and lessons learned from, out-of-hospital cardiac arrest missions during the COVID-19 pandemic: An interview study. Nordic Journal of Nursing Research. 2024 Feb;44.
11 Republic of the Philippines - Department of Education. IMPLEMENTING RULES AND REGULATIONS OF REPUBLIC ACT NO. 10871 (An Act Requiring Basic Education Students to Undergo Age-Appropriate ' Basic Life Support Training), DepEd Order No. 054 S. 2021. 9 Dec 2021. Available from: https://www.deped.gov.ph/wp-content/uploads/2022/01/DO_s2021_054.pdf.
12 European Society of Cardiology. Resuscitation in out-of-hospital cardiac arrest – it’s how quickly it is done, rather than who does it [Internet]. France: European Society of Cardiology; 2025 Mar 14 [cited 27 Jun 2025]. Available from: https://www.escardio.org/The-ESC/Press-Office/Press-releases/resuscitation-in-out-of-hospital-cardiac-arrest-it-s-how-quickly-it-is-done-r.
13 Strnad M, Borovnik Lesjak V, Jerot P, Esih M. Prehospital Predictors of Survival in Patients with Out-of-Hospital Cardiac Arrest. Medicina (Kaunas). 2023 Sep 26;59(10):1717.
14 Han Y, Hu H, Shao Y, Deng Z, Liu D. The link between initial cardiac rhythm and survival outcomes in in-hospital cardiac arrest using propensity score matching, adjustment, and weighting. Sci Rep. 2024 Apr 1;14(1):7621.
15 Kandori K, Nakajima S, Matsuyama T, Kitamura T, Narumiya H, Hitosugi M, et al. Association Between No-Flow Time, Prehospital Low-Flow Time, and Conversion to Nonshockable Rhythm in Patients With Out-of-Hospital Cardiac Arrest Presenting With Initial Shockable Rhythm: A Nationwide Prospective Study in Japan. J Am Heart Assoc. 2025 Mar 4;14(5):e038725.
16 Brooks SC, Clegg GR, Bray J, Deakin CD, Perkins GD, Ringh M, et al. Optimizing Outcomes After Out-of-Hospital Cardiac Arrest With Innovative Approaches to Public-Access Defibrillation: A Scientific Statement From the International Liaison Committee on Resuscitation. Circulation. 2022 Mar 29;145(13):e776-e801.
17 Ombay G. Cardiologists seek law mandating AEDs in public spaces. 2024 May 28 [cited 2025 Jun 27]. In. GMA News Online [Internet]. Quezon: GMA News Online; c2025. Available from: https://www.gmanetwork.com/news/topstories/nation/908243/cardiologists-seek-law-mandating-aeds-in-public-spaces/story/.
18 AED Rescue Philippines. Metro Manila law enforcement on the deployment of AED at establishments [Internet]. Manila: AED Rescue Philippines; c2018. Available from: https://www.aedrescuephilippines.com/aed-metro-manila-law-enforcement.
19 Vu DH, Hoang BH, Do NS, Do GP, Dao XD, Nguyen HH, et al. Why Bystanders Did Not Perform Cardiopulmonary Resuscitation on Out-of-Hospital Cardiac Arrest Patients: A Multi-Center Study in Hanoi (Vietnam). Prehosp Disaster Med. 2022 Feb;37(1):101-105.
20 UnitekEMT. Rural vs. Urban: Differences in EMT Responses and Resources [Internet]. Phoenix: Unitek EMT. 2024 Jul 25 [cited 27 Jun 2025]. Available from: https://www.unitekemt.com/blog/rural-vs-urban-differences-in-emt-responses-and-resources/.
21 Chua ISY, Fook-Chong SMC, Shahidah N, Ng YY, Chia MYC, Mao DR, et al. The association between mode of transport and out-of-hospital cardiac arrest outcomes in Singapore. Resuscitation. 2022 Apr;173:136-143.
22 Ageta K, Naito H, Yorifuji T, Obara T, Nojima T, Yamada T, et al. Delay in Emergency Medical Service Transportation Responsiveness during the COVID-19 Pandemic in a Minimally Affected Region. Acta Med Okayama. 2020 Dec;74(6):513-520.
23 Satty T, Ramgopal S, Elmer J, Mosesso VN, Martin-Gill C. EMS responses and non-transports during the COVID-19 pandemic. Am J Emerg Med. 2021 Apr;42:1-8.
24 Renkiewicz GK, Hubble MW, Wesley DR, Dorian PA, Losh MJ, Swain R, et al. Probability of a shockable presenting rhythm as a function of EMS response time. Prehosp Emerg Care. 2014 Apr-Jun;18(2):224-30.
25 Ono Y, Hayakawa M, Iijima H, Maekawa K, Kodate A, et al. The response time threshold for predicting favourable neurological outcomes in patients with bystander-witnessed out-of-hospital cardiac arrest. Resuscitation. 2016 Oct;107:65-70.
26 Pu Y, Chai X, Yang G. Association between prehospital time and in-hospital outcomes in out-of-hospital cardiac arrests according to resuscitation outcomes consortium epidemiologic registry. Heart Lung. 2024 Mar-Apr;64:168-175.
27 Goniewicz M, Bednarz K, Al-Wathinani AM, Goniewicz K. Assessment of Emergency Medical Service (EMS) response times and operational factors in out-of-hospital cardiac arrests (OHCA): a retrospective analysis. Postepy Kardiol Interwencyjnej. 2025 Mar;21(1):25-36.
28 Hayashi M, Iwasaki YK. Addressing out-of-hospital cardiac arrest with current technology advances: Breaking the deadlock with a mobile network. J Arrhythm. 2024 Jul 4;40(4):753-766.
29 Cardiac Arrest Registry to Enhance Survival (CARES). 2021 Annual Report. Incidence and demographic. 2021.
30 Hawkes C, Booth S, Ji C, Brace-McDonnell SJ, Whittington A, Mapstone J, et al. Epidemiology and outcomes from out-of-hospital cardiac arrests in England. Resuscitation. 2017 Jan;110:133-140.
31 Beck B, Bray J, Cameron P, Smith K, Walker T, Grantham H, et al. Regional variation in the characteristics, incidence and outcomes of out-of-hospital cardiac arrest in Australia and New Zealand: Results from the Aus-ROC Epistry. Resuscitation. 2018 May;126:49-57.
32 Mawani M, Kadir MM, Azam I, Mehmood A, McNally B, Stevens K, et al. Epidemiology and outcomes of out-of-hospital cardiac arrest in a developing country-a multicenter cohort study. BMC Emerg Med. 2016 Jul 28;16(1):28.
33 Horriar L, Rott N, Böttiger BW. Improving survival after cardiac arrest in Europe: The synergetic effect of rescue chain strategies. Resusc Plus. 2023 Dec 21;17:100533.

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Authors who publish with this journal agree to the following terms:
- Authors retain copyright and grant the journal right of first publication with the work simultaneously licensed under a Creative Commons Attribution-NonCommercial 4.0 International License that allows others to share the work for non-commercial purposes with an acknowledgement of the work's authorship and initial publication in this journal.
- Authors are able to enter into separate, additional, non-commercial contractual arrangements for the non-exclusive distribution of the journal's published version of the work (e.g., post it to an institutional repository or publish it in a book), with an acknowledgement of its initial publication in this journal.
- Authors grant the journal permission to rewrite, edit, modify, store and/or publish the submission in any medium or format a version or abstract forming part thereof, all associated supplemental materials, and subsequent errata, if necessary, in a publicly available publication or database.
- Authors warrant that the submission is original with the authors and does not infringe or transfer any copyright or violate any other right of any third parties.