Clinical features
The lesion started as a papule on the dorsal surface of his left foot fifteen years prior to consultation. The lesion gradually increased in size and was later associated with pain and swelling. The patient also noticed that the swelling discharged pus and pale granular material. He tolerated the condition, until seven years prior to the consultation, when he was admitted to their local hospital, where debridement was performed. Three years prior to the present consultation, he sought care at the Surgery Department of this institution. A biopsy performed showed acute and chronic inflammation with abscess formation. He was prescribed unrecalled medications, but his condition did not improve. He was subsequently referred to the Orthopedics Department for transfer of service, and then to our department for co-management.The patient is a farmer who works in the crop fields. He does not have diabetes or any autoimmune disease and has no family history of mycetoma. He has been a smoker for eleven pack-years and is an occasional alcoholic beverage drinker. He denied any previous trauma or injury to the affected foot and reported no travel to mycetoma-endemic areas. The patient had no fever, dyspnea, or other associated systemic conditions.
On cutaneous examination, the patient had a non-tender, subcutaneous, indurated mass on the dorsal surface of the left foot, measuring 15 × 10 cm (Figure 1). The mass contained multiple plaques with hard, woody swelling, discharging sinuses, and white or pale grains, each measuring 1 to 2 mm (Figure 2). Inguinal lymphadenopathy was palpated on the left side. Physical examination findings of the right leg and foot were unremarkable. Based on the patient’s history and physical examination, we made an initial diagnosis of Madura foot.
Diagnostics, therapeutics, and outcomes
A magnetic resonance imaging done revealed a soft tissue mass in the medial plantar region of the left foot, with infiltration of the deep plantar muscles, suggestive of plantar fibromatosis. The patient was subsequently admitted for open biopsy with intraoperative frozen section biopsy of the left foot mass, which showed myxoid tissue with chronic inflammation and fibrous tissue with abscess formation. Blood tests were unremarkable except for anemia (hemoglobin: 88 g/L) and thrombocytosis (platelet count: 768 × 10³/μL). Radiographic examination of the left foot showed irregular osseous lucencies in the metatarsals and calcaneus with overlying tissue swelling suggestive of osteomyelitis. Wound gram stain and bacterial culture, acid fast bacilli, and KOH were all negative.Tissue and white or pale grain samples were analyzed for bacterial and mycological evaluation. Direct microscopy was positive for pale grains. Fungal culture was negative. At this point, we were considering the diagnosis of a probable actinomycetoma. We prescribed oral co-amoxiclav initially for two weeks, with a plan to continue it for up to six months, and advised the patient to follow-up after two weeks or earlier if grains appeared in the discharge. We requested a repeat fungal culture, but the patient refused.
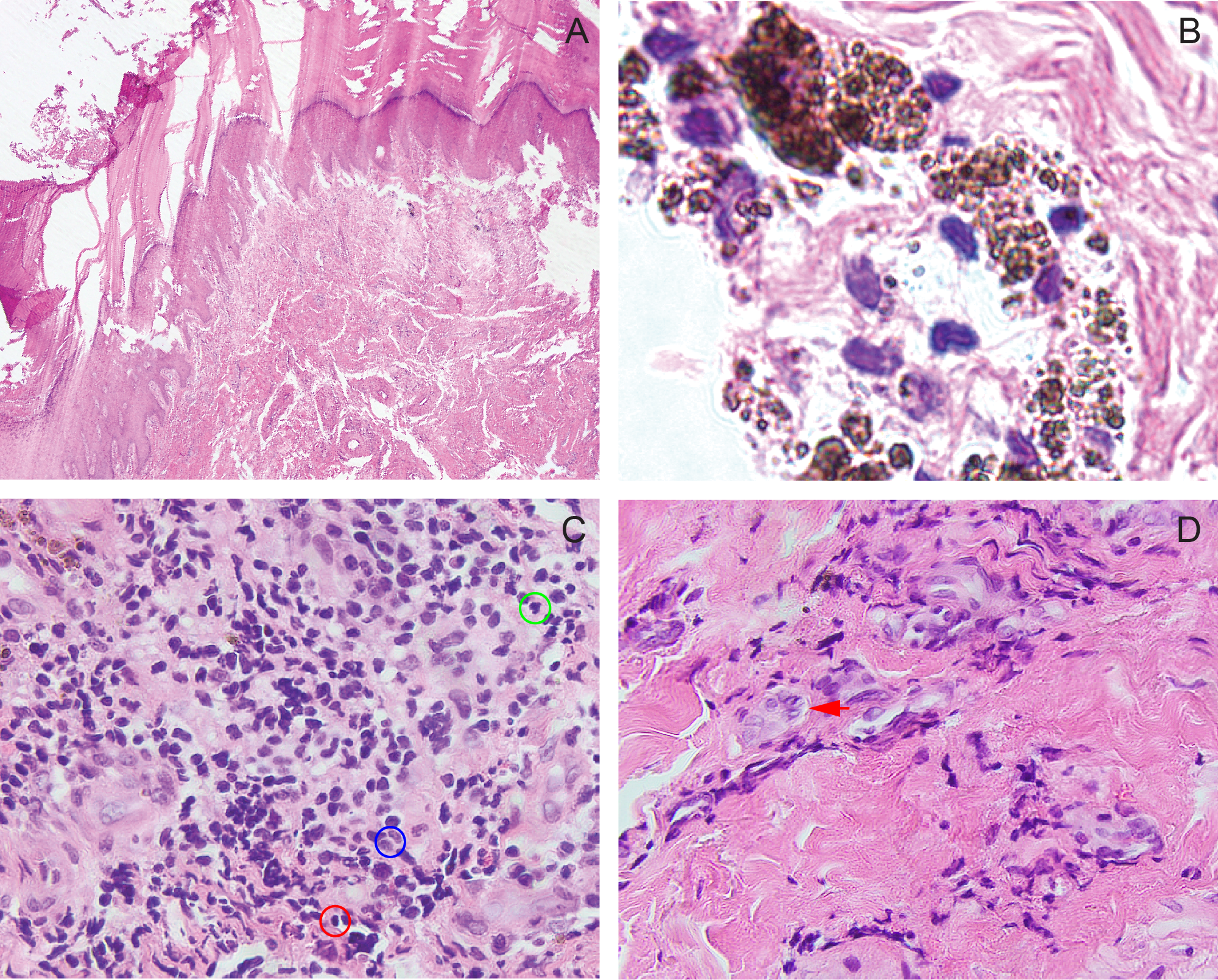
The patient was lost to follow-up for four years, until he was admitted to our institution, with pneumonia, pulmonary tuberculosis, and type 2 diabetes mellitus. At the ward, we performed another wedge incision biopsy. Histopathology revealed thick orthokeratotic bands overlying an acanthotic epidermis. The superficial dermis contained multiple melanophages and mild to moderately dense interstitial inflammatory infiltrates composed predominantly of lymphocytes, histiocytes, neutrophils, and numerous fibroblasts. Foreign body giant cells were also present. These findings indicated granulomatous and suppurative dermatitis. (Figure 3). Periodic acid-Schiff (PAS) stain was positive for fungal hyphae, which supports the diagnosis of eumycetoma. We then immediately started the patient on itraconazole at 200 mg/day for six months, with planned surgical debridement thereafter. However, the patient reported poor compliance to the antifungal medication. Concurrently, he was placed on a six-month course of antitubercular therapy. In the fifth month of treatment, he developed severe pain and swelling of the left foot. The Orthopedics service admitted the patient and subsequently performed a below-the-knee amputation.
Relevance
Madura foot, also knon as mycetoma, is a chronic, progressive granulomatous inflammatory reaction caused by fungi (eumycetoma) or anaerobic filamentous bacteria (actinomycetoma). It involves the skin, subcutaneous tissue, muscles, joints, and bones, leading to deformities of the hands, feet, or legs. The global burden of mycetoma is unknown,1 but in the Philippines, incidence is 0.10 per 100,000 annually.2 3 Eumycetoma accounts for 40% of global cases, while actinomycetoma comprises 60%.4 5Mycetoma predominantly occurs in male rural workers residing in subtropical and tropical regions who come into direct contact with contaminated soil. Diagnosis can be made by the classic clinical triad of a painless hard subcutaneous mass, sinus tracts, and pathognomonic grains (microcolony aggregates) in the discharge.6 7 8 Direct microscopy, cytological, histopathological, and immunohistochemical examinations, as well as grain culture, help identify the causative agent. On histopathology and cytology, the color of the grains helps differentiate between eumycetoma and actinomycetoma. The presence of the black grains points to eumycetoma, while yellow to brown or red to pink grains indicate actinomycetoma. Pale, white, or yellow grains, on the other hand, may be seen in both types of mycetoma.9
In our patient, eumycetoma was diagnosed based on clinical presentation and histopathological findings on hematoxylin-eosin and PAS stains. Fungal culture, in combination with internal transcribed spacer region gene amplification, is a key tool in identifying the causative agent of eumycetoma.10 11 The distinction between eumycetoma and actinomycetoma is crucial, as their treatments differ significantly. Eumycetoma may be refractory to medical treatment and often requires surgical intervention. Actinomycetoma generally responds well to long-term antimicrobial therapy.12
In our patient's case, the painless nature of his symptoms led to a delay in seeking medical attention, resulting in progressive foot swelling. The severe pain and swelling he experienced 21 years after symptom onset and during the fifth month of antitubercular therapy--were attributed to mass effect from significant inflammation and edema, ultimately necessitating emergency leg amputation. Given the diagnostic and therapeutic challenges associated with eumycetoma, this case underscores the critical need for early diagnosis and treatment to achieve better patient outcomes.