Clinical profile of pediatric patients with COVID-19 admitted to Southern Philippines Medical Center before vaccine rollout
SPMC J Health Care Serv. 2025;11(1):2 ARK: https://n2t.net/ark:/76951/jhcs8kwt35
Rica Marie B Andico,1 Ameleen B Bangayan,1 Jo-Anne J Lobo1
1Department of Pediatrics, Southern Philippines Medical Center, JP Laurel Ave, Davao City, Philippines
Correspondence Rica Marie B Andico, rica_andico@yahoo.com
Received 28 February 2024
Accepted 13 March 2025
Cite as Andico RMB, Bangayan AB, Lobo JJ. Clinical profile of pediatric patients with COVID-19 admitted to Southern Philippines Medical Center before vaccine rollout. SPMC J Health Care Serv. 2025;11(1):2. https://n2t.net/ark:/76951/jhcs8kwt35
Prior to the availability of COVID-19 vaccines, global reports indicated that children accounted for a small percentage of confirmed cases,
1 with lower rates of severe illness and better prognosis compared to adults.
1 Several theories have been proposed to explain these differences, including the underdeveloped angiotensin-converting enzyme 2 (ACE2) receptors in children, created competition with other viral infections, and a more active immune response.
2 However, pediatric patients still presented a range of clinical manifestations, with fever and cough being the most common symptoms.
During the peak of the COVID-19 pandemic, the Southern Philippines Medical Center (SPMC) served as the primary referral hospital for patients with COVID-19 in Davao City. In 2020, SPMC had admitted about 5,050 COVID-19 cases. Despite this, a comprehensive profile of pediatric patients diagnosed with COVID-19 remains lacking. Understanding their demographic and clinical characteristics is essential, given the unique physiological and immunological factors influencing disease susceptibility and severity in children.
This study aims to describe the demographic and clinical profile of pediatric patients admitted to SPMC for COVID-19 infection prior to the introduction of COVID-19 vaccines, providing baseline data for future comparisons in the post-vaccination era.
We did a descriptive research among pediatric patients with confirmed COVID-19 infection based on reverse transcription polymerase chain reaction (RT-PCR) testing who were subsequently admitted to the Department of Pediatrics in Southern Philippines Medical Center (SPMC) from 1 March 2020 up to 28 February 2021. Medical records of these pediatric patients were reviewed, and data on sociodemographic and clinical profiles--including age, sex, place of residence (within or outside Davao City), nutritional status (normal, stunted, wasted, overweight, or obese), comorbidities (cardiovascular, gastrointestinal, hematologic, metabolic, neurologic, oncologic, renal, and/or respiratory conditions)--were recorded. Data on COVID-19 characteristics, such as disease severity (asymptomatic, mild, moderate, severe, or critical), presenting signs and symptoms (ageusia, altered mental state, anorexia, anosmia, coryza, cough, diarrhea, dyspnea, fever, nausea and vomiting, myalgia, sore throat, and others), initial diagnostic tests performed (complete blood count, C-Reactive Protein (CRP) test, and chest x-ray), and clinical outcomes (length of hospital stay and disposition), were also recorded.
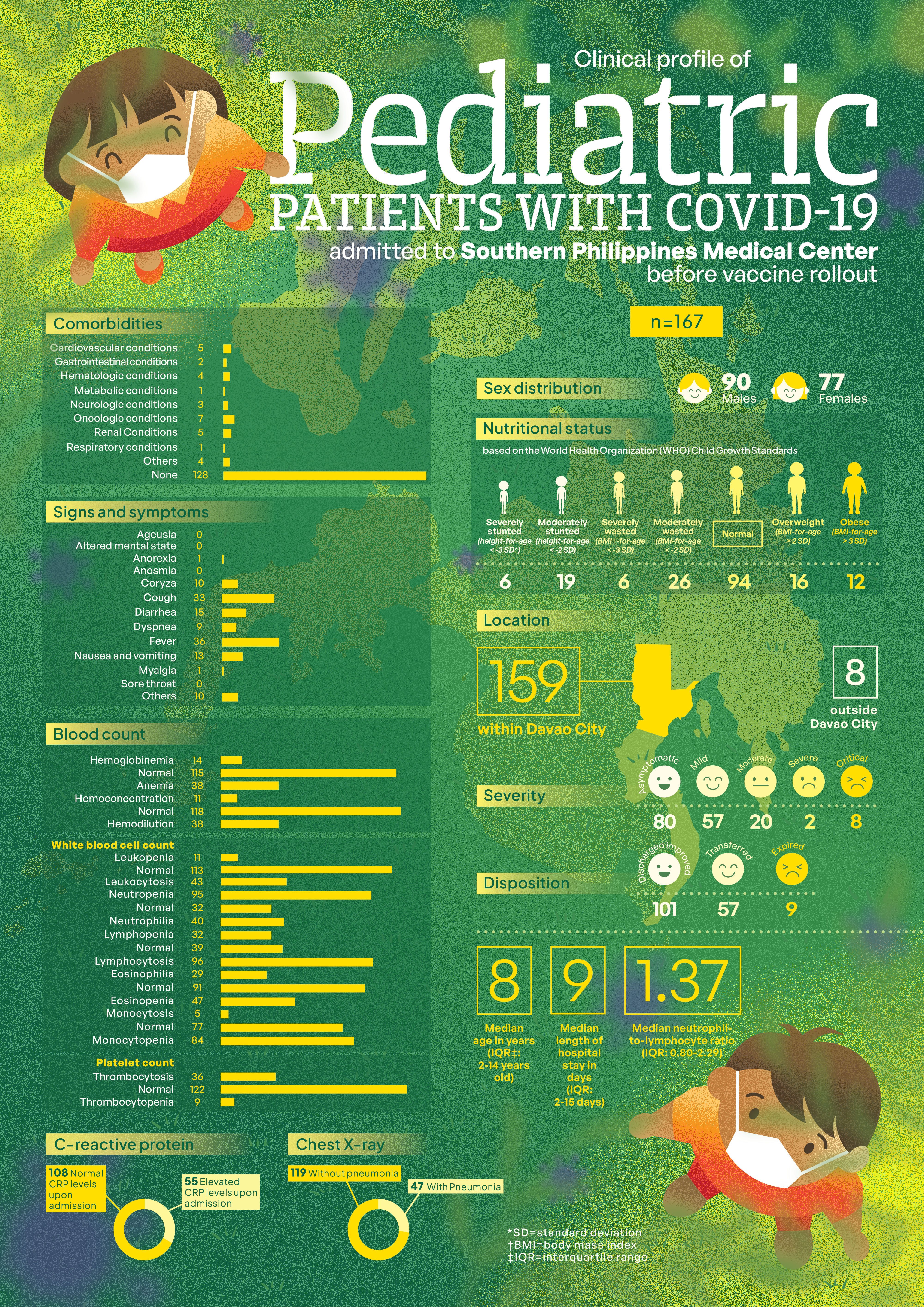
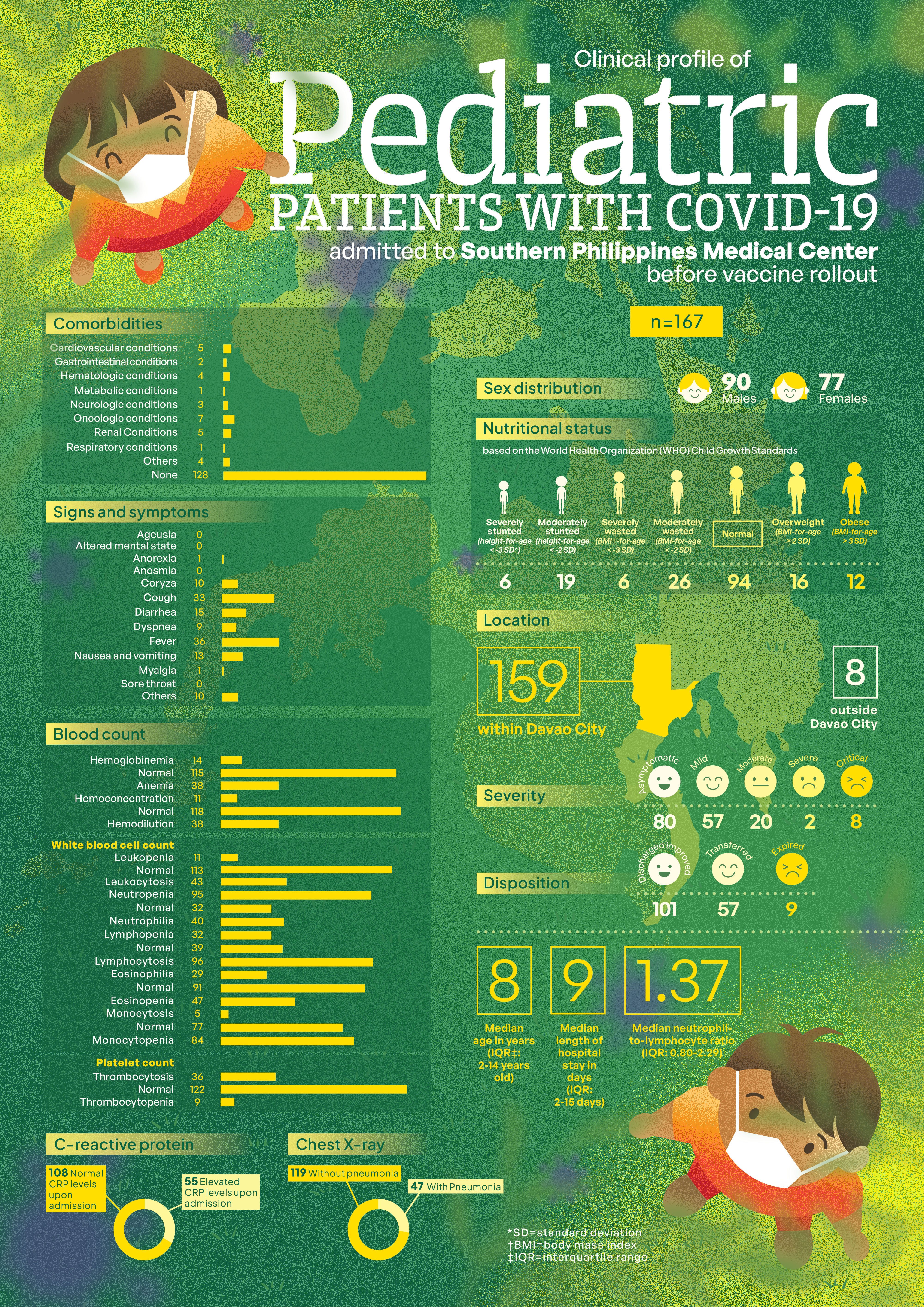
From a total of 668 pediatric patients with COVID-19 infection, we selected 167 patients for inclusion in this study through systematic sampling. The median age of patients upon admission for COVID-19 infection was 8 years (IQR: 2-14 years), with a sex distribution of 90/167 (53.89%) males, and 77/167 (46.11%) females. Most patients resided within Davao City (159/167; 95.21%). Of the 167 patients assessed, 94 (56.29%) had normal nutritional status. Based on the World Health Organization (WHO) Child Growth Standards, 19/167 (5.39%) were moderately stunted (height-for-age < -2 SD) and 6/167 (3.59%) were severely stunted (height-for-age < -3 SD). In terms of wasting, 26/167 (15.57%) were moderately wasted (BMI-for-age < -2 SD) and 6/167 (3.59%) were severely wasted (BMI-for-age < -3 SD). Additionally, 16/167 (9.59%) were classified as overweight (BMI-for-age > 2 SD), and 12/167 (7.23%) were classified as obese (BMI-for-age > 3 SD). Among the 167 patients, 5 (2.99%) had cardiovascular conditions, 7 (4.19%) had oncologic conditions, and 5 (2.99%) had renal conditions.
Most patients were asymptomatic or had mild symptoms (137/167; 82.03%), while the rest had moderate, severe, or critical symptoms. Unlike adult patients with COVID-19 infection, pediatric patients in this study did not present with ageusia, anosmia, and/or sore throat. Most patients presented with cough (33/167; 19.76%) and fever (36/167; 21.56%). Chest x-ray results showed that 47/167 (28.31%) had pneumonia upon admission for COVID-19 infection.
Upon admission, most patients had a normal hemoglobin count (115/167; 68.86%), while some had anemia (38/167; 22.75%), and the rest had hemoglobinemia (14/167; 8.38%). In terms of hematocrit, most patients also had normal hematocrit count (118/167; 70.66%), followed by hemodilution (38/167; 22.75%), and the rest had hemoconcentration (11/167; 6.59%). Most patients also had a normal white blood cell count (113/166; 67.66%), while a smaller percentage had leukocytosis (43/167; 25.75%), and an even smaller percentage had leukopenia (11/167; 6.59%). The median neutrophil-to-lymphocyte ratio (NLR) was 1.37 (IQR: 0.80 to 2.29). Over half of the patients had neutropenia (95/167; 56.89%), lymphocytosis (96/167; 57.49%), monocytopenia (84/167; 50.60%), and normal eosinophil count (91/167; 54.49%). However, a significant number of patients also had eosinopenia (47/167; 28.14%). Most patients had normal platelet count (122/167; 73.05%), while 55/163 (33.74%) had elevated CRP levels upon admission.
The median length of hospital stay was 9 days (IQR: 2-15 days), with most patients in improved condition (101/167; 60.48%) upon discharge.
Our study provides a comprehensive overview of the demographic and clinical profiles of admitted pediatric patients with COVID-19 infection prior to the vaccine rollout, revealing more favorable outcomes than those reported in adults. Unlike adults, who commonly presented with ageusia, anosmia, and sore throat, our pediatric patients were mostly asymptomatic or exhibited only mild symptoms. While adult cases often showed lymphopenia and neutropenia, children in our study had lymphocytosis and neutrophilia, although white blood cell counts were normal in both groups. Platelet counts were generally normal in most patients, but thrombocytopenia occurred in more severe cases, mirroring adult patterns. These findings highlight the distinct clinical profile of COVID-19 infection in pediatric patients.
Contributors
RMBA, ABB and JJL contributed to the conceptualization of this article. All authors wrote the original draft, performed the subsequent revisions, approved the final version, and agreed to be accountable for all aspects of this report.
Acknowledgments
Our sincerest gratitude to the Department of Pediatrics in Southern Philippines Medical Center for their steadfast guidance and support throughout this research. Despite the challenges of the pandemic, we persevered—always in service of the Filipino children.
Ethics approval
This study was reviewed and approved by the Department of Health XI Joint Research Ethics Committee (DOH XI JREC reference JREC-202256).
Competing interests
None declared
Access and license
This is an Open Access article licensed under the Creative Commons
Attribution-NonCommercial
4.0 International License, which allows
others to share and adapt the work, provided that derivative works
bear appropriate citation to this original work and are not used for
commercial purposes. To view a copy of this license, visit
https://creativecommons.org/licenses/by-nc/4.0/.
References
1. Hon KLE, Leung KKY. Pediatric COVID-19: what disease is this? World J Pediatr. 2020 Aug;16(4):323-325.
2. Tiruneh FT. Clinical Profile of Covid-19 in Children, Review of Existing Literatures. Pediatric Health Med Ther. 2020 Sep 21;11:385-392.
Copyright © 2025 RMB Andico, et al.